Credentialing Process at Novita
There are various steps involved in the complete credentialing and contracting process. Every step is very important and should be managed very carefully as any errors can lead to a longer credentialing process and can result in heavy financial loss for the provider/practice. Our expert with 15 years of insurance relationship management experience will help you sail through the difficult steps with ease.

Get Ready for The Future, Today!
Credentialing and contracting are the basis of starting a clinic or healthcare facility. It sets the foundation for how your practice is going to do in the future years.
The healthcare organization and provider cannot be paid by that carrier for services rendered unless they are properly credentialed. Each insurance carrier has a unique credentialing process and every physician in your practice will need to go through the medical credentialing process for that carrier before claims can be processed. Any clerical error or missing information may cause the credentialing to be declined. That scenario can lead to a longer wait time for payment of services and, in some cases, may mean that payments will not be honored by the insurance carrier. Physicians cannot be granted privileges in most healthcare organizations without first completing the medical credentialing process.
Request a free evaluation of your practice from our financial consultants.
Benefits of Novita Credentialing Service
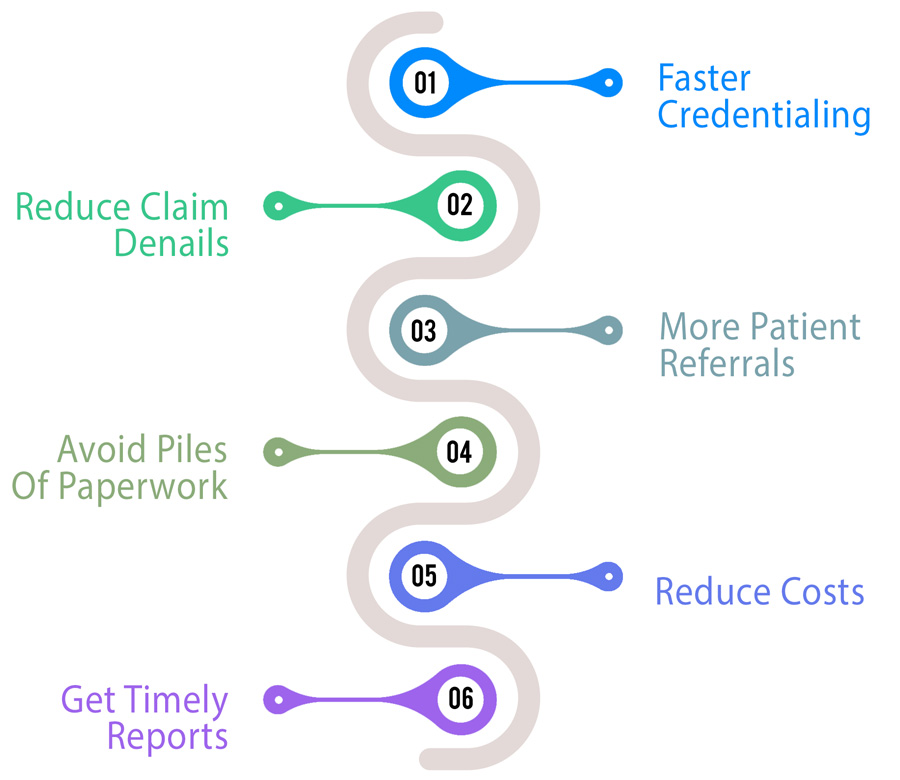
With our diligent credentialing and Enrollment services, you get the following benefits:
o Get credentialed faster with all significant payers
o Reduce claim denials and improve cash flow
o Get more patient referrals from the network
o Avoid piles of paperwork with our document management system
o Get support for filling up cumbersome application forms
o Reduce costs of the credentialing process with our global delivery teams
o Get timely reports on the status of your applications
We have helped many providers and practices with the initial credentialing, re‐credentialing, and getting the best out of
their practices.
What Novita Offers
We start with the first step and collect all the required information and documents to file applications. The information and documents are provided by the provider or practice. The documentation requirements vary from payer by payer.
New Credentialing
- Medicare Individual Credentialing
- Medicare Group Credentialing
- Individual providers benefit reassignment to group
- Medicaid Individual Credentialing
- Medicaid Group Credentialing
- Individual and Group Credentialing with Commercials
Contracts Creation and Maintenance
-
New Group/Individual Practitioner contracts
-
Adding / Deleting providers in the existing contract
-
Adding/Deleting location in the current contract
-
Adding / Deleting plan types ( Line of Business ) in the current contract
CAQH Attestation
-
CAQH application filing
-
CAQH quarterly attestations
-
Expirations and Renewals
-
The tracking expiry date for State DEA License, Board certificate, and Malpractice Insurance
Provider Data Maintenance – Update Management on Payer Systems
- Provider demographic update in payers file.
- Provider directory maintenance on payer websites.
- EFT/ERA enrollments
Tracking and Analytics
- Maintaining a repository of provider’s credentialing documents
- Maintaining Contracting agreements
- Tracking credentialing dates, expiration, and alerting dates to initiate credentialing processes
- Working with the denials team to understand if there are any claim denials due to credentialing issues
Numbers & Achievements
We did awesome work with business ethics.

15
Years of Experience

99
% First Pass Rate

15
% Revenue Increase

100
% Coding Compliance
Get started with Novita
Get in touch with us today to get better contracted rates. Get Quick Quote.
Physician Credentialing FAQs
It helps to ensure that healthcare facilities only contract with qualified and competent physicians to provide patient care.
Physician information such as education, training, work history, license, and insurance details are typically required for credentialing.
They streamline the credentialing process, reduce administrative burdens, ensure compliance with regulations, and provide a secure and centralized database of physician information.
Hospitals, clinics, private practices, and other healthcare facilities use physician credentialing services to manage the credentialing process for their contracted physicians.




