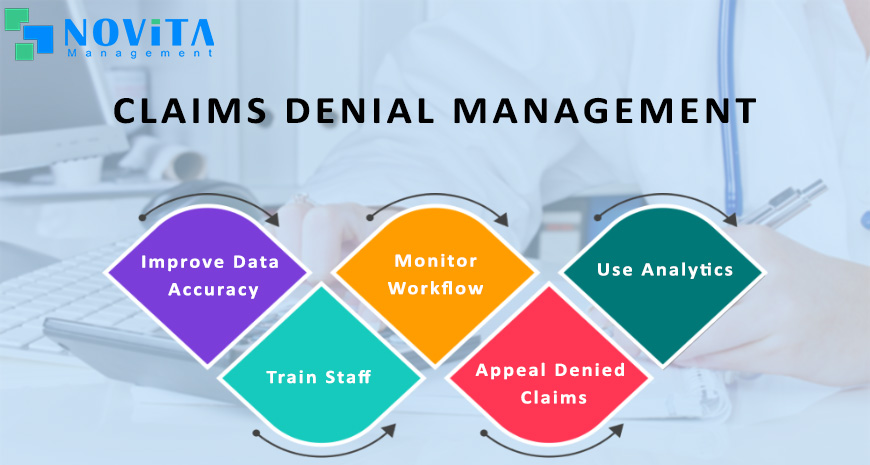
Effective claims denial management is essential for healthcare providers and organizations to maximize revenue and minimize financial losses. Here are some steps you can take to improve your claims denial management process:
- Analyze denial trends: Start by analyzing your denial data to identify trends and patterns. This can help you understand the root causes of denials and develop strategies to address them. Use your data to determine the most common reasons for denials, such as missing or incorrect information, coding errors, or lack of documentation.
- Improve data accuracy: Ensure that all the data you submit on claims is accurate and complete. This includes patient demographics, insurance information, and medical codes. Implementing electronic health records (EHRs) and claims management software can help improve data accuracy and reduce errors.
- Train staff: Provide training to staff members responsible for claim submission and denial management. This includes educating them on proper coding and billing procedures, as well as the importance of accurate documentation. Make sure they are up-to-date on any changes in insurance policies, billing codes, or regulations that may affect your claims process.
- Monitor workflow: Monitor your claims process to identify bottlenecks and inefficiencies that may contribute to denials. Streamline workflows and implement automation where possible to improve efficiency and accuracy.
- Appeal denied claims: Develop a system for timely and effective appeals of denied claims. This may involve developing a standardized process for documenting and appealing denials, as well as tracking and monitoring the progress of appeals.
- Use analytics: Use analytics to track and monitor key performance indicators (KPIs) related to claims management, such as denial rates, denial reasons, and time to resolution. Use this data to identify areas for improvement and measure the effectiveness of your denial management strategies.
By implementing these steps, you can improve your claims denial management process and reduce revenue loss due to denials or you can hire Novita Management Services team to help you with denials management and prevention.
